Latest Updates
The first-ever Women's Vascular Summit was held in April 2019 by vascular surgeons at the University at Buffalo's Jacobs School of Medicine and Biomedical Sciences. Participants came from all over the country. The organizers of the conference realized that writing a book about women's vascular health was a necessary next step after those discussions were so fruitful.
The end result is "Women's Vascular Disease: An Overview of the Literature and Treatment Recommendations" Caitlin W. Hicks, MD, associate professor of surgery at Johns Hopkins University School of Medicine, and Linda M. Harris, MD, professor of surgery in the Jacobs School and program director of UB's vascular surgery residency, are the editors of the book.
The book is partly based on the contributions of all female panelists at the 2019 conference. Other surgeons who are interested in how sex affects vascular disease also contributed to the book.
The book as well as the conference, which has been held twice now (the most recent time was virtually in April), aim to better inform medical professionals about the differences in women's vascular disease presentation and outcomes and to highlight the issues that will increase the likelihood of a diagnosis and the right treatment.
According to Harris, a vascular surgeon at UBMD Surgery, "I want clinicians to start thinking about vascular disease in women, to understand that many women do have vascular disease, but their presentation is not going to be textbook." I want them to know that if a woman presents with symptoms, they should think about testing her because her presentation won't be typical, unlike that of a man, whose symptoms are typically based on how men present."
For instance, one of the subjects that the book delves into is the possibility that a woman who suffers a stroke will exhibit distinct symptoms in comparison to a man.
According to Harris' explanation, "it may not be weakness in an arm or leg as it might be in a man, but may present differently at first, such as a sudden memory issue, and the clinician may not be expecting that"
Harris added that women may develop vascular disease later than men typically do, making them more vulnerable and affecting their symptoms. She said that doctors need to know that women may have aneurysms in different parts of their bodies than men do in order to make these diagnoses more quickly. The potentially lethal bulging of an artery wall is known as an aneurysm.)
According to Harris, "Prevention and screening in women should also be considered." According to the recommendations of the Society for Vascular Surgery, women who smoke or have a family history of aneurysms should be considered for screening. This has not typically been done because vascular disease was incorrectly assumed to be less common in women.
The book also talks about how issues of race and culture, like unconscious bias, affect how women with vascular disease show up and are diagnosed.

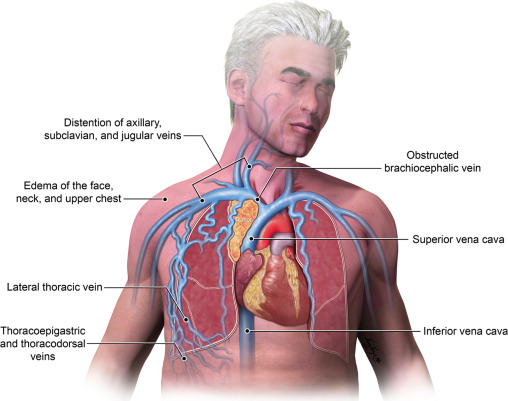
Occupations of blood vessels in the human circulatory system have the potential to cause serious issues, similar to a water line that has become blocked. This is especially true in the condition known as superior vena cava syndrome (SVCS), in which the heart is prevented from receiving oxygen-depleted blood that comes from the upper chest, arms, and head. SVCS, on the other hand, necessitates immediate attention and is far more serious than the inconvenience of low water pressure caused by a clogged pipe.
Around 15,000 people in the United States suffer from SVCS each year, which can cause mental confusion, facial swelling, difficulty breathing, chest pain, and even coma. The condition can be caused by intravascular devices like pacemakers and catheters that may compress or obstruct the superior vena cava vessel, although the most common cause is a tumor.
SVCS has historically been treated with radiation therapy, which kills tumor cells. However, in recent years, minimally invasive endovascular stenting, in which a tubular support is inserted into the collapsed or obstructed vessel, has emerged as the standard of care of choice. Endovascular therapy is currently the safest and most effective treatment for SVCS, according to a new analysis by researchers at Temple University's Lewis Katz School of Medicine. Previously, it was unknown whether it was the best option.
For older obese adults, cutting 250 calories a day while engaging in moderate exercise yielded greater benefits than exercise alone. According to new research published today in the flagship journal of the American Heart Association, Circulation, combining aerobic exercise with a moderate reduction in daily calories led to greater improvements in aortic stiffness—a measure of vascular health that has an impact on cardiovascular disease—in older adults who were obese.
Age-related increases in aortic stiffness may be offset by modifiable lifestyle factors like eating a healthy diet and engaging in regular physical activity. Previous research has demonstrated that, despite the fact that aerobic exercise generally has positive effects on the structure and function of the aorta, exercise alone may not be sufficient to reduce aortic stiffness in obese older adults.
This randomized, controlled trial included 160 obese, sedentary adults between the ages of 65 and 79 with BMIs between 30 and 45 kg/m2. The participants were, on average, 69 years old; 74% were women; and 73% were white. For 20 weeks, participants were placed in one of three intervention groups at random: 1) They only exercise and eat as usual; 2) Regular exercise combined with a moderate calorie restriction (about 250 calories per day) or 3) a combination of exercise and stricter calorie restriction (about 600 fewer calories per day).
Pre-prepared meals with less than 30% fat and at least 0.8 grams of protein per kilogram of ideal body weight were provided to the two calorie-restricted groups for the study by a registered dietitian. They created their own breakfasts using the menu that the dietitian recommended. During the 20-week study at Wake Forest School of Medicine's Geriatric Research Center, each participant received supervised aerobic exercise training four days per week.
